Publication Highlight Catheter Management After Benign Transurethral Prostate Surgery: RAND/UCLA Appropriateness Criteria Ted A. Skolarus, Casey A. Dauw, Karen E. Fowler, Jason D. Mann, Steven J. Bernstein and Jennifer Meddings THE AMERICAN JOURNAL OF MANAGED CARE, December 2019
Benign prostatic hyperplasia (BPH) is a leading diagnosis among males. Approximately 100,000 men are treated with transurethral prostate (TURP) surgery each year, making it one of the most common surgical procedures in the United States and several other countries.
TURP routinely involves urinary catheter placement, but there are no guidelines for the duration of urinary catheter use after prostate surgery. Given an increasing focus on appropriateness of care for policy, payment, quality, and patient-centered care, clarifying appropriate urinary catheter duration could help improve consistency and quality of care for healthcare organizations and their patients treated surgically for BPH.
Some providers recommend overnight urinary catheter placement, whereas others recommend leaving the catheter in place for days afterward. Several studies have shown that decreasing indwelling urinary catheter duration not only reduces patient discomfort and nursing care during hospitalization and after discharge, but it also lowers the risks of complications, including catheter-associated urinary tract infections (UTIs).
In the absence of evidence-based guidelines, defining the most appropriate duration of urinary catheter use after this common procedure may help decrease practice variation, reduce postoperative complication risk, and improve consistency and quality of care for patients with BPH and lower urinary tract symptoms.
In the current publication, Skolarus et al assessed the appropriateness of different timings of urinary catheter removal among patients after prostate surgery. Both the use of intermittent catheterization (IC) as well as indwelling urethral catheters were evaluated.
A literature review was conducted to identify the most relevant articles assessing outcomes for patients undergoing TURP. Following the RAND/UCLA Appropriateness Method* a multidisciplinary panel of 11 experts and practicing urologists were asked to review these studies and use their clinical expertise to rate the appropriateness of different options for urinary catheter removal and trial of void after BPH surgery.
In total 44 articles were included, and the expert panel rated them for appropriateness of urinary catheter use and urinary retention. The expert panel examined appropriateness across 4 clinical scenarios (no preexisting catheter, preexisting catheter [including intermittent], difficult catheter placement, significant perforation) and 5 durations (postoperative day [POD] 0, 1, 2, 3-6, or ≥7).
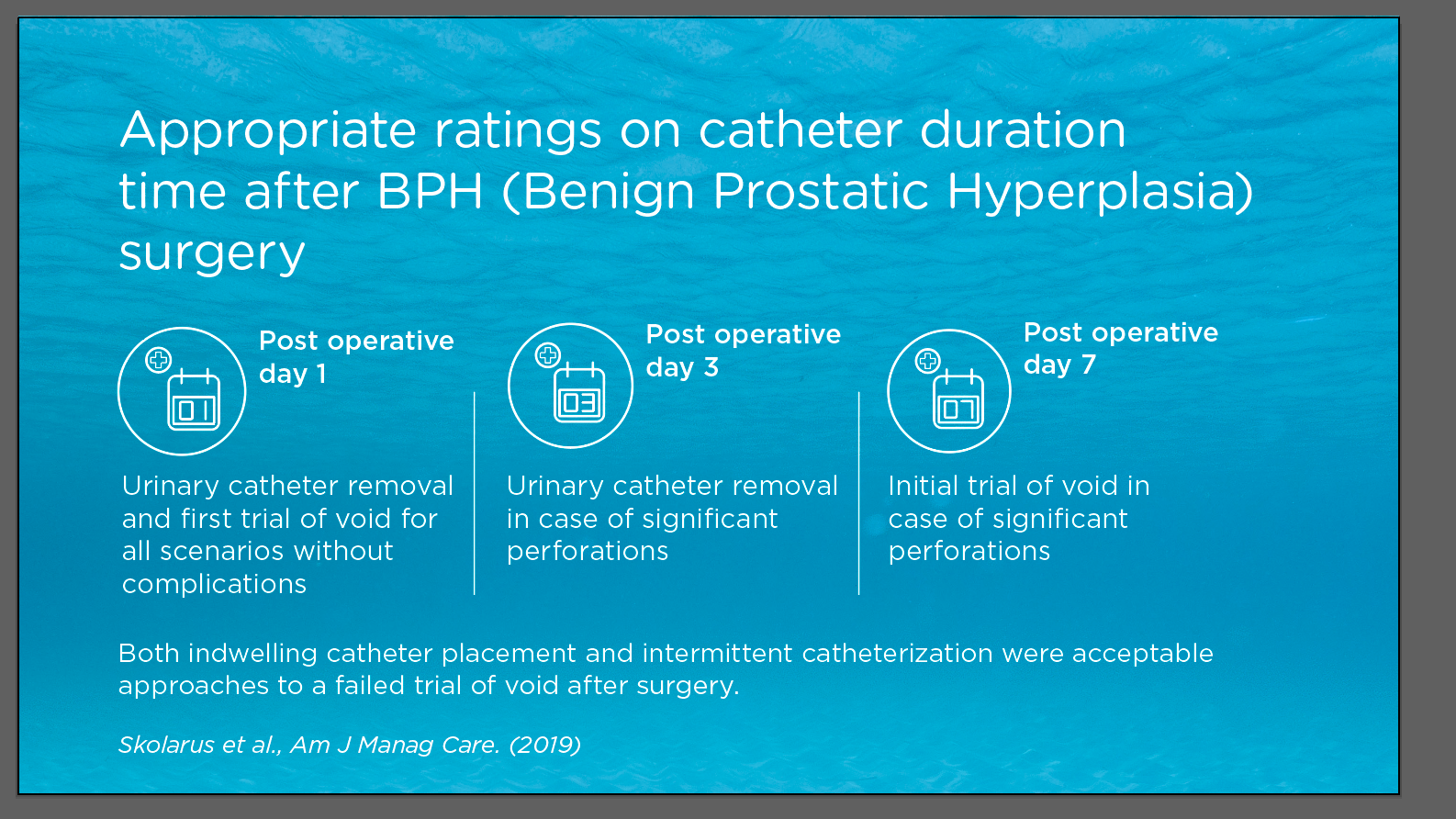
Based on the panel ratings, urinary catheter removal and first trial of void on the first day after surgery was appropriate for the majority of patients and waiting more than 3 days was linked to health issues.
However, in case of complications, e.g. clinically significant perforations, waiting 3 days after the surgery was deemed the earliest appropriate timing for removal. The perforation scenario was the only appropriate indication for waiting 7 or more days for initial trial of void.
The expert panel was asked to rate how appropriate urinary catheterization is to manage retention if failing the first trial of void after surgery, both IC and/or indwelling urethral catheter were in scope.
The panel uniformly rated both IC and indwelling urethral catheter placement as appropriate.
If a Foley catheter was placed after a failure of first trial to void post-surgery, the expert panel rated a second trial of void appropriate after 1 or 2 days in hospitalized patients. For patients discharged home, waiting up to 4 days was the longest appropriate duration per the expert panel, with waiting 5 to 7 days for a second trial of void rated as uncertain or raising disagreement among the panelists.
The duration of catheter use after surgery is poorly understood and standardizing postoperative catheter use is likely to decrease practice and length of stay variation, minimize catheter discomfort for patients, and potentially lower the risk of postoperative complications (e.g. UTI). The lack of quality indicators for transurethral prostate surgery is striking given the variation in practice across hospitals. The publication by Skolarus et al provides recommendations from practicing clinicians as a potential initial quality measure to promote consistent, appropriate care for men surgically treated for BPH. There is an interest by the Centers for Disease Control and Prevention (CDC), which collects measures of catheter-associated UTI and catheter use, in developing a measure of urinary catheter appropriateness that could be applied based on data from the electronic health record (e.g. procedure type, comorbidity).
Conclusions
Skolarus et al defined clinically relevant guidance statements for the appropriateness of catheter duration after transurethral prostate surgery. Findings from this robust methodological approach, including urethral catheter removal and trial of void the first day after surgery being rated as appropriate for all scenarios except clinically significant perforations, may help promote the consistency and quality of care for patients undergoing transurethral surgery for BPH within and across healthcare delivery systems.
* The RAND/UCLA Appropriateness Method (RAM) was developed in the mid 1980s, as part of the RAND Corporation/University of California Los Angeles (UCLA) Health Services Utilisation Study, primarily as an instrument to enable the measurement of the overuse and underuse of medical and surgical procedures