Bowel control
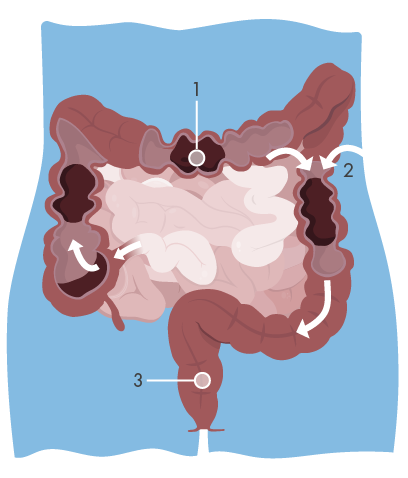 The descending colon and the rectum are the final stage of the human intestine system. Normally the rectum is relatively empty. Stools do not enter the rectum continuously, but as mass movements. These movements are often started by gastro-colic response. Food arriving in the stomach sets off a pressure wave in the colon and starts major waves of pressure. Often large amounts of the contents of the colon arrive in the rectum at once. As filling of the rectum continues, nerve impulses are dispatched to the cerebral cortex resulting in awareness of the need to defaecate.
The descending colon and the rectum are the final stage of the human intestine system. Normally the rectum is relatively empty. Stools do not enter the rectum continuously, but as mass movements. These movements are often started by gastro-colic response. Food arriving in the stomach sets off a pressure wave in the colon and starts major waves of pressure. Often large amounts of the contents of the colon arrive in the rectum at once. As filling of the rectum continues, nerve impulses are dispatched to the cerebral cortex resulting in awareness of the need to defaecate.
Defaecation
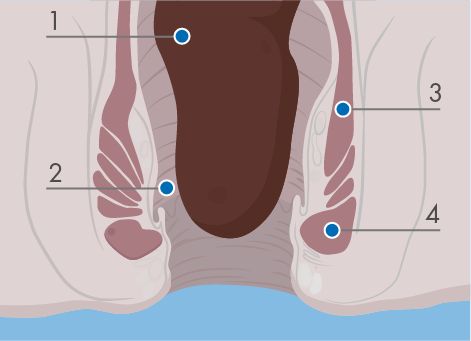 When stool enters the rectum the internal anal sphincter muscle automatically relaxes and opens up the top of the anal canal. Around the internal anal sphincter is the external anal sphincter, which contracts automatically when the stool arrives. This is the muscle around the anus that you can deliberately squeeze. If evacuation of stool at that time is possible, the sphincter becomes voluntarily relaxed and pressure in the sphincter is reduced. Contraction of the diaphragm and abdominal muscles raise intra-abdominal pressure and trigger peristalsis in the colon and rectum, the internal sphincter relaxes and when the rectal pressure exceeds the sphincter pressure, defaecation occurs.
When stool enters the rectum the internal anal sphincter muscle automatically relaxes and opens up the top of the anal canal. Around the internal anal sphincter is the external anal sphincter, which contracts automatically when the stool arrives. This is the muscle around the anus that you can deliberately squeeze. If evacuation of stool at that time is possible, the sphincter becomes voluntarily relaxed and pressure in the sphincter is reduced. Contraction of the diaphragm and abdominal muscles raise intra-abdominal pressure and trigger peristalsis in the colon and rectum, the internal sphincter relaxes and when the rectal pressure exceeds the sphincter pressure, defaecation occurs.
The bowel’s intrinsic nervous system
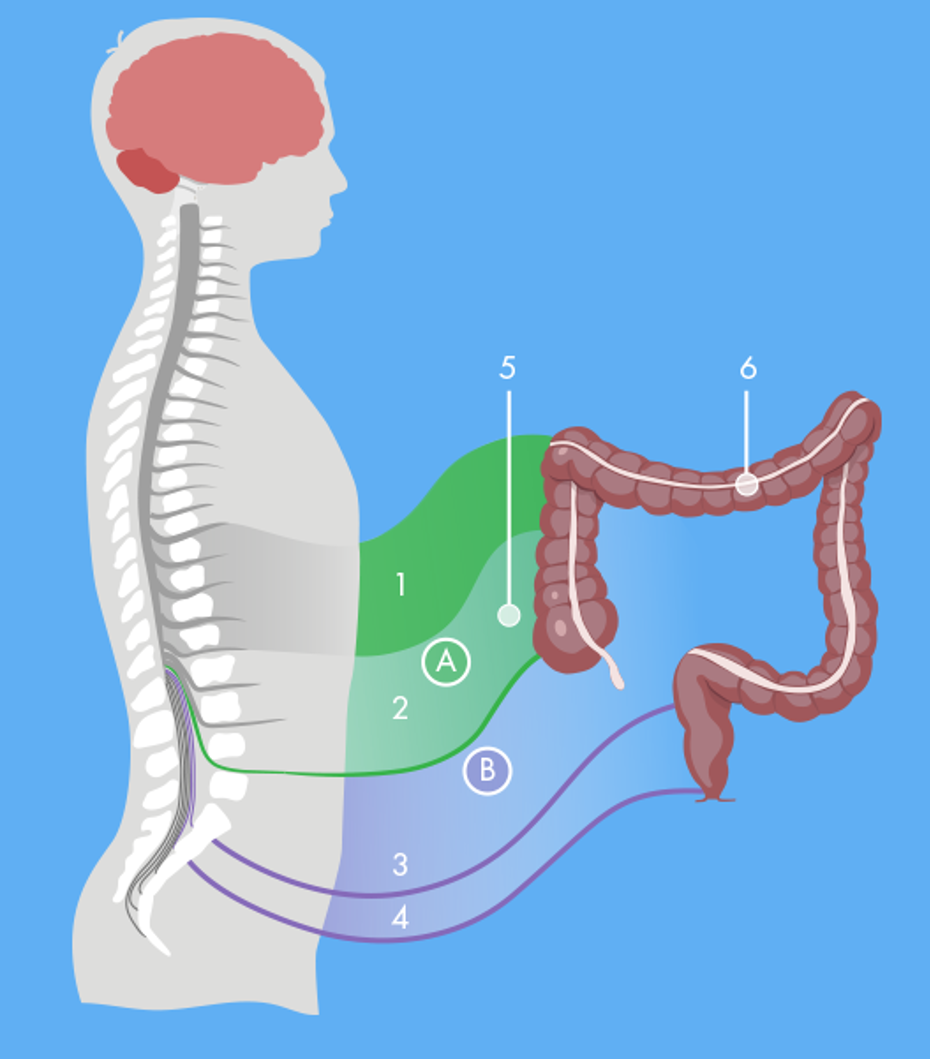
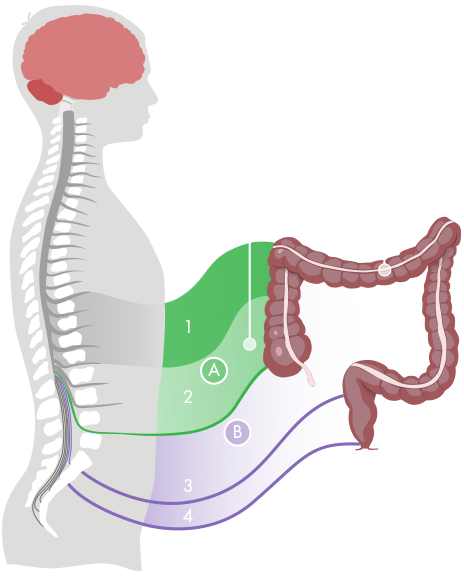
The bowel wall has an intrinsic nervous system which coordinates gut secretion, blood flow and muscular activity. It can function without extrinsic nerve signals, although in an uncoordinated fashion. Extrinsic innervation comes from the parasympathetic and sympathetic nervous systems, which are parts of the autonomous nervous system.
The sympathetic and parasympathetic nervous system
The parasympathetic nervous system stimulates motility and is connected to the bowel and the bladder through nerves at the sacral region of the spinal cord. The sympathetic nervous system inhibits motility and is connected to the bowel through the mesenteric nerves and the hypogastric nerves at the sacral region. These nerves also control the bladder. That is why many people with NBD not only have problems with defaecation, but also a dysfunctional bladder. The ascending colon and around two thirds of the transverse colon are innervated by the parasympathetic nerves from between the S1 and L5 vertebrae. The left part of the colon and rectum are innervated by the pelvic nerves. The anal region is innervated by the pudendal nerves.
What is NBD?
The everyday definition of neurogenic bowel dysfunction (nbd) is when the bowel doesn’t work properly due to loss of normal sensory or motor control, or both, as a result of central neurological disease or damage. Damage to the spinal cord or brain interrupt the neural pathways and the problems will vary depending on the severity and location of the damage. The reduced bowel management can lead to constipation, faecal incontinence and/or disordered defecation. Many patients spend a considerable amount of time trying to manage this problem.