Learn more about what cauda equina syndrome is, its effects on bladder and bowel, and how to manage bladder and bowel symptoms in cauda equina.
What is cauda equina syndrome?
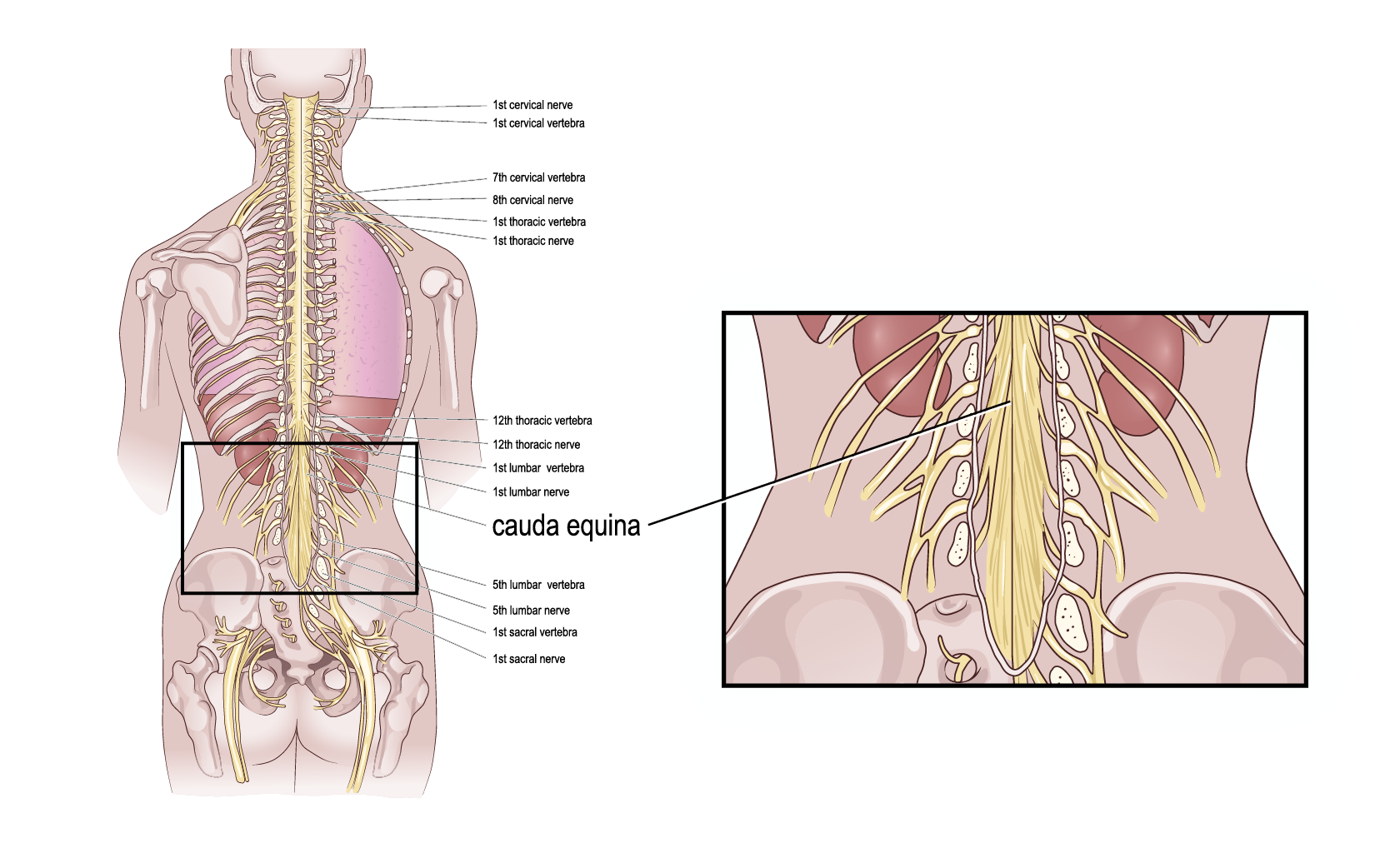
Cauda equina syndrome (CES) is a condition that affects the bundle of nerves located at the lower end of the spinal cord, called the cauda equina (latin for horse’s tail). This bundle of nerves is part of what controls the bladder, bowel, and sexual function as well as the lower limbs. When these nerves become compressed or damaged, it can lead to various symptoms like:
- Saddle anesthesia – reduced or loss of feeling around the buttocks, anus and genitals
- Pain – severe pain in the back and/or down in one or both legs
- Incontinence – bladder and/or bowel incontinence, or inability /difficulty to pass urine and/or constipation
- Numbness in the legs – lack of or altered sensation and/or weakness in the legs
The onset of the symptoms may be gradual or rapid. If there is sudden onset of symptoms, it is classed as a medical emergency that requires surgical intervention. Early CES signs are change in bladder and bowel control such as changes in urine stream or inability to fully empty the bladder or bowel. The symptoms of CES can be nearly similar to symptoms of Sciatica and it is therefore commonly mistaken for it. To diagnose CES medical imaging such as an MRI or CT scan is required for confirmation.
What causes cauda equina syndrome?
The cause of CES varies, but it is usually when there is a disc herniation in the lower part of the back that compresses the nerves. The compression or damage to the nerves may also be caused by spinal stenosis, tumor, trauma, inflammatory / infectious conditions or due to a complication after a medical intervention such as surgery.
Bladder and bowel function in cauda equina syndrome
One of the significant effects of cauda equina syndrome is its impact on bladder and bowel function. The compression or damage to the nerves can disrupt the normal communication between the brain, spinal cord, and the bladder and bowel, resulting in incontinence or difficulties emptying.
Bladder Dysfunction: CES can lead to urinary retention or difficulty in emptying the bladder completely. This occurs because the nerves responsible for controlling bladder function may be affected. Patients may experience symptoms such as:
· a weak urinary stream
· difficulty initiating urination
· difficulty to fully emptying the bladder causing urine retention
· need to stand, strain, or press on the bladder to urinate
· the sensation of incomplete emptying
· reduced sensation in the bladder making it hard to tell when the bladder is full
In severe cases, the bladder can overfill, causing urinary incontinence or the inability to urinate at all.
Bowel Dysfunction: Similarly, CES can affect the nerves that control bowel movements, leading to bowel dysfunction. The disruption of nerve signals can impair the normal contraction and relaxation of the muscles in the rectum and anus, making it challenging to have regular bowel movements. Patients may experience:
· constipation
· difficulty passing stool
· inability to control bowel movements (fecal incontinence)
How is cauda equina syndrome managed?
As a healthcare professional, it's important to be aware of CES and its potential impact on bladder and bowel function. By recognizing the symptoms, communicating with the medical team, and providing appropriate care and support, nurses can help facilitate the best possible outcomes for patients with this condition.
Early diagnosis and treatment are crucial to preventing long-term complications, including permanent bladder and bowel dysfunction. Treatment for CES typically involves surgical decompression to relieve the pressure on the affected nerves. In some cases, patients may require additional treatments, such as physical therapy, to regain strength and function in the affected areas. Rehabilitation and ongoing management, such as intermittent catheterization and transanal irrigation, may be necessary to address any long-term bladder and bowel issues that persist after treatment.
An effective bladder and bowel management regime enables improved quality of life. Intermittent catheterization (IC) is an option for bladder management that can help with emptying the bladder completely, avoiding residual urine that can cause recurrent urinary tract infections and leakage of urine.
In a clinical study, transanal irrigation (TAI), also called bowel or rectal irrigation, has been shown to be an effective bowel management choice for patients with CES compared to previous bowel management, which were digital stimulation and manual evacuation. The conclusion from the clinical study is that this non-pharmaceutical method of bowel management is effective and has the potential to improve symptoms of bowel dysfunction.