Pelvic floor dysfunction is common, but not commonly talked about. Pelvic floor issues resulting in bladder and/or bowel incontinence evoke a heightened sense of taboo and embarrassment, surpassing that experienced with other medical conditions. Not talking about the issues, or getting the help needed, can lead to social isolation that is associated with a significant impact on mental health and wellbeing. Therefore, it is important to discuss both bladder and bowel issues with patients. In this article, you will find an explanation of basic pelvic floor anatomy, and a description of symptoms and how these can be managed, which can be downloaded and handed out to your patients.
Pelvic floor dysfunction – how to managing your bladder and bowel symptoms
The pelvic floor’s main function is to support your bladder, urethra, vagina, uterus, bowel, rectum and anus. There are a number of reasons that the muscles in the pelvic floor can be weakened or damaged causing pelvic floor dysfunction. Pelvic floor dysfunction is a collection of different conditions that refers to the inability to correctly relax and/or coordinate your pelvic floor muscles. It commonly affects your bladder and bowel with symptoms like:
- frequent need to urinate
- having bladder or bowel urgency - having to rush to get to the toilet
- having bladder or bowel leakage
- difficulties emptying the bladder or bowel
The bladder and bowel are closely related and can affect each other. If you experience constipation this can make it harder to completely empty the bladder.
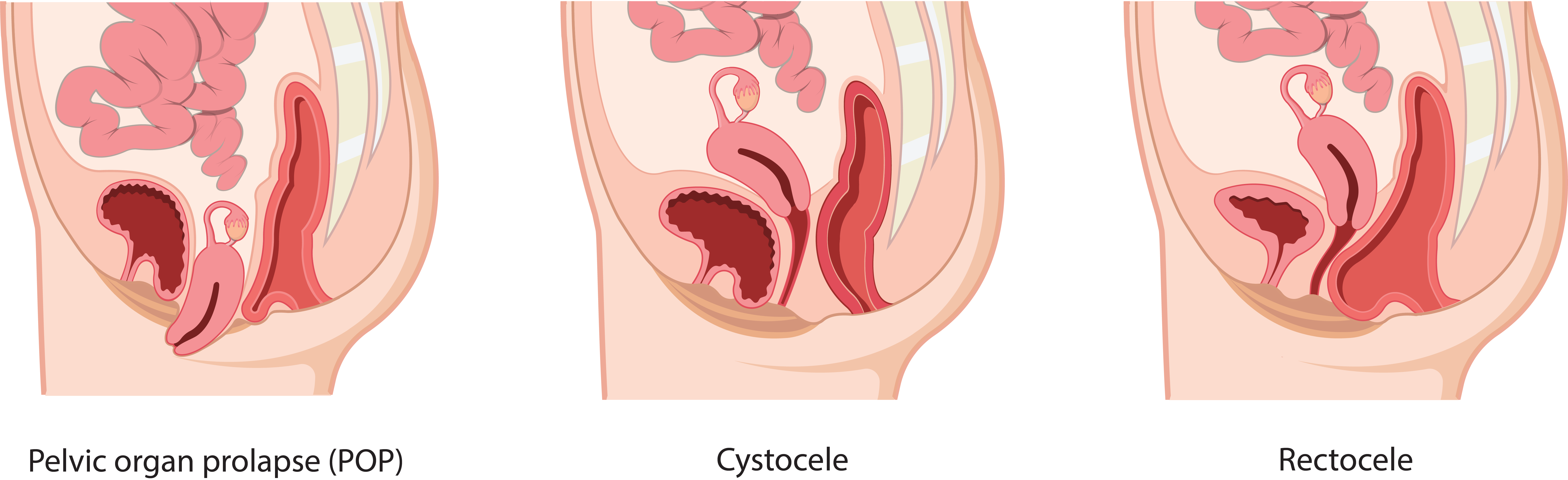
Pelvic organ prolapse (POP) is when one or more of the organs supported by your pelvic floor has moved or slipped out of its normal position due to weakened or damaged tissue and muscles.
Cystocele occurs when supportive tissue around the bladder and vaginal wall weakens and stretches, allowing the bladder to push the front wall of the vagina backwards.
Rectocele is when the rectum bulges against the posterior vaginal wall that traps stool and makes emptying of the bowel difficult.
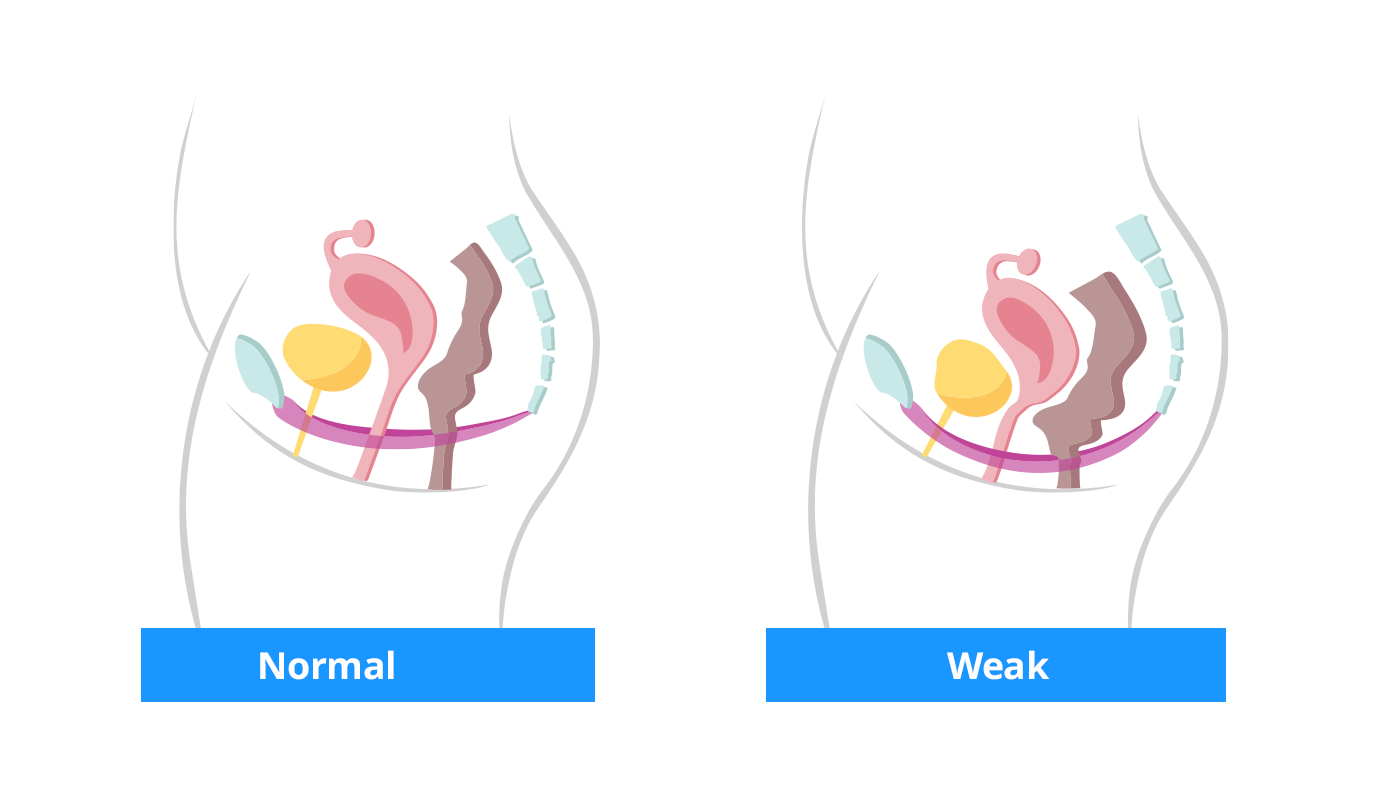
Female anatomy: In the first image is a healthy pelvic floor that supports the bladder, uterus and bowel, and in the second image, is a weakened pelvic floor causing the organs to move or slip out of its normal position.
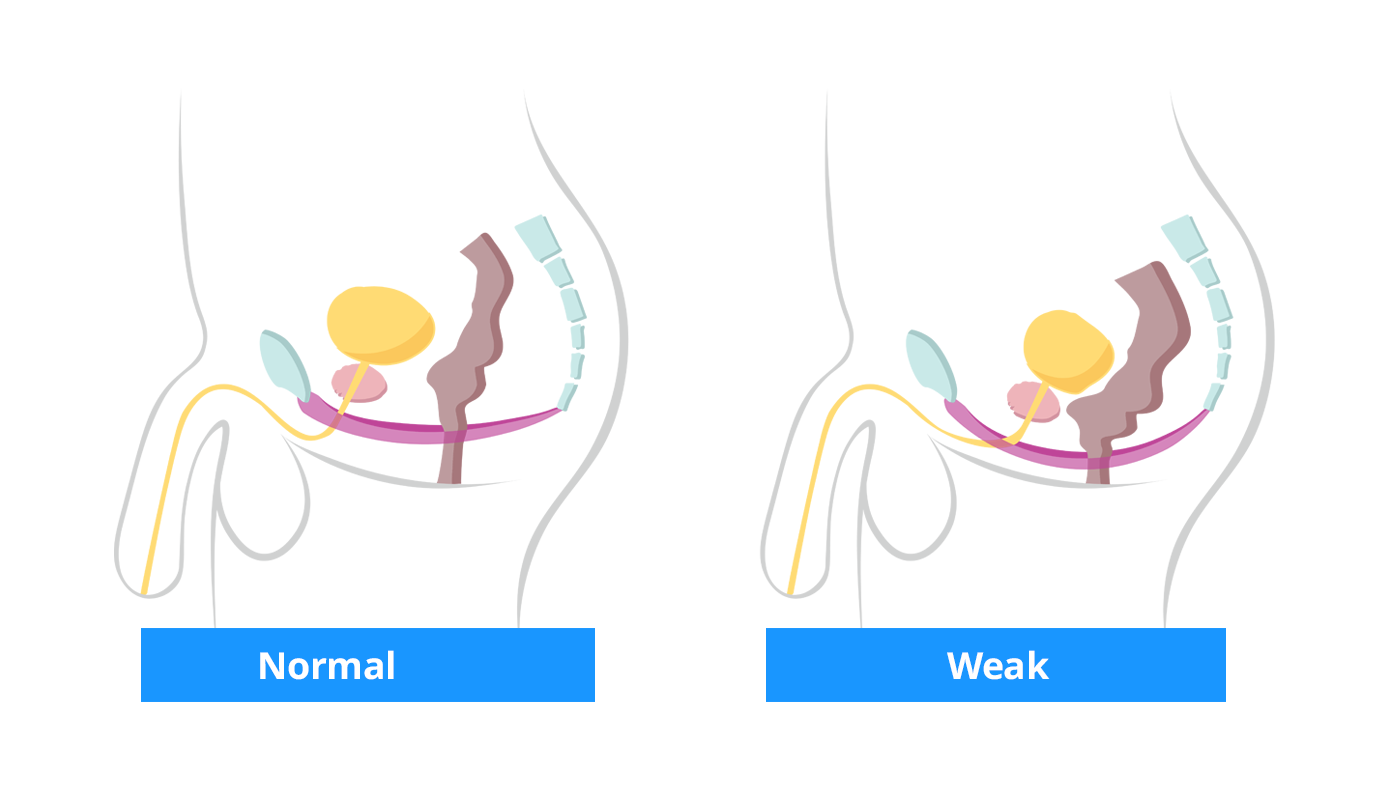
Male anatomy: In the first image is a healthy pelvic floor that supports the bladder and bowel, and in the second image, is a weakened pelvic floor causing the organs to move or slip out of its normal position.
Talk to your doctor
A good way to describe your symptoms is to use a bladder and/or bowel diary and to prepare for your visit by answering following questions:
- How many times do you empty your bladder daily?
- Do you feel that you completely empty your bladder each time?
- How many times per day/per week do you empty your bowels?
- Do you feel that you completely empty your bowel each time?
- Do your bladder/bowel issues limit your daily activities?
- Do you assist emptying such as with your finger, pressing, toilet position?
- Do you experience any pain for instance during sexual activity?
Remember to have a list of your medications to hand, as these may affect the bladder and bowel.
How to manage pelvic floor symptoms?
Initial treatments are lifestyle modifications, physical therapy and/or biofeedback.
Pelvic floor symptoms such as an overactive bladder or incomplete emptying of the bowel typically stay or become worse if they are not managed. Instead of living with pain and discomfort, you can improve your everyday life by using aids to assist emptying of your bladder and bowel such as intermittent catheterisation and bowel irrigation.
Intermittent catheterisation (IC) is a treatment option when you have:
- the inability to pass urine (urine/urinary retention)
- Incomplete bladder emptying
- very slow or intermittent stream
- problems with urinary tract infections as a result of incomplete emptying of your bladder
- a urethral stricture – narrowing of the bladder outlet tube
Intermittent catheterisation is considered the gold standard of manually draining urine from your bladder when this does not occur naturally. Your doctor or nurse will train you on the IC process and it involves placing a small tube (catheter) in the bladder to empty the urine. You do this periodically, often 4-6 times a day. By keeping to your schedule, you can reduce leakage, and the risk of infection, and protect your bladder.
Bowel irrigation, also called transanal irrigation (TAI), is a treatment option when you have:
- bowel leakage or fear of leakage
- a feeling something is left and have an urge to try to empty your bowel often
- need to use your fingers to assist emptying
- having difficulties to start or finish emptying and need to excessively strain
- use mini enemas with laxatives every day and you don’t feel good about it
Bowel irrigation is a way to assist emptying of your bowel by instilling water through your anus. The water helps to empty your rectum and soften the stool. Your doctor or nurse will train you and give you advice on the amount of water you need and how often you should use it depending on your bowel issues. Once a routine is established you can reduce the risk of leakage, be in control of when and where to empty your bowel and reduce the feeling of incomplete emptying.