This is a short summary of the article by Shaman Rajindrajith, Niranga Manjuri Devanarayana, and Marc A Benninga in World Journal of Clinical Pediatrics, 2022 September 9; 11(5): 385-404
Chronic constipation in children is common with a global prevalence of 9.5% and in the review written by Rajindrajith et al, the authors share their view of childhood constipation based on a critical review of the available literature. Paediatric constipation is an important health problem with a high impact on the quality of life of the affected child and their family. The healthcare costs of constipation in children are large due to repeated hospital admissions, emergency room visits, and regular clinic visits. A better understanding of the management of constipation could reduce healthcare costs.
What is paediatric functional constipation?
Functional constipation is characterised by infrequent and painful bowel movements, faecal incontinence, stool withholding behavior, and occasional passage of large diameter stools. Functional constipation is common, and the causes could vary, the main pathophysiology mechanisms according to the authors are stool withholding and colonic and anorectal dysfunction. This could be due to different risk factors and there are several risk factors described in the review such as:
- stressful life event
- abuse and child maltreatment
- psychological and behavioral factors
- toilet training
- lifestyle, such as diet and physical activity
- abnormal microbiota
- pathophysiology, such as altered sensation
Why is it important to manage constipation in children?
Children with constipation have a low quality of life, with pain during defaecation, abdominal discomfort due to faecal impaction, and associated faecal incontinence causing embarrassment and shame. If the constipation is left untreated or is poorly managed the child tends to have significant complications and it is therefore important to manage constipation at the early stages to relieve symptoms.
Apart from the high impact on the child’s health-related quality of life, there are burdens of healthcare costs. Faecal impaction and abdominal pain are common reasons for emergency room visits, management with medications and regular clinic visits, methods to investigate with anorectal and colonic manometry, and in refractory cases, surgical interventions - all contributing to the cost of constipation.
In the review the authors describe that a thorough clinical evaluation, understanding of physiology, colonic and anorectal function are needed for diagnosis of functional constipation. There are some prognostic factors that have a negative impact on treatment success. It is important that these factors are assessed and are part of the decision making for therapeutic options:
- constipation during the 1st year of life
- longer duration of symptoms before presentation
- low defaecation frequency at presentation
- presence of faecal incontinence
- large diameter stools
- stool withholding
- night time urinary incontinence
- presence of faecal mass in the bowel
- prolonged colonic transit (>100 h)
- failed balloon expulsion test
How to relieve constipation in children?
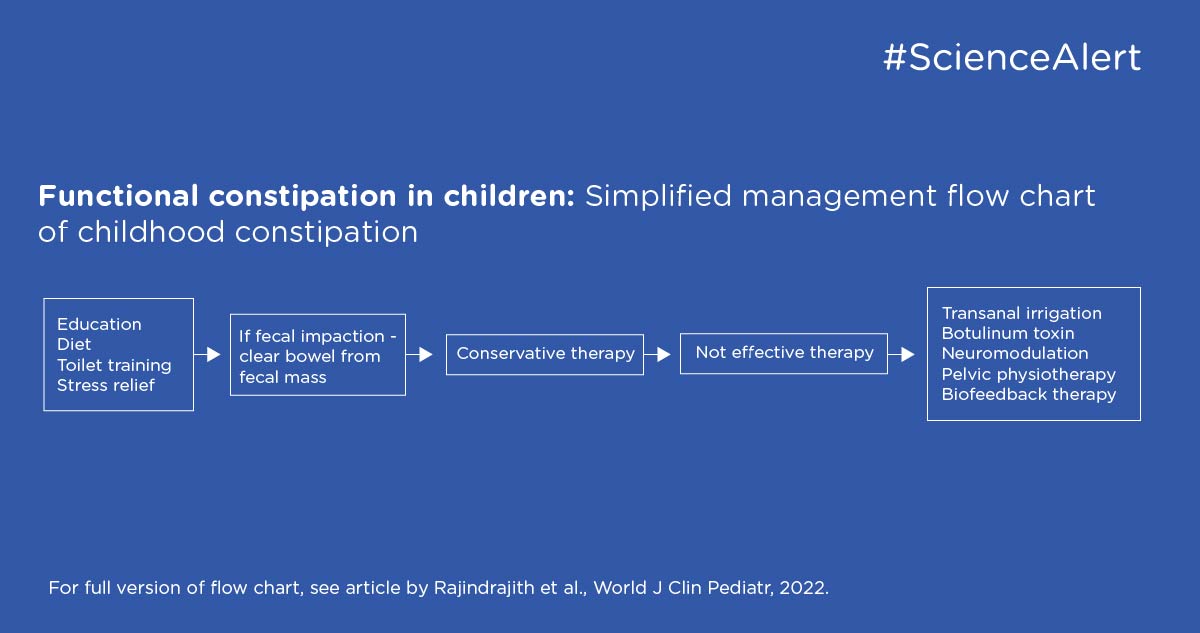
The first step is usually to clear up the rectum and colon since most children with constipation will have faecal impaction. This is important since the response to the drugs commonly used to manage constipation can be affected by the faecal mass. If no faecal impaction or effective clearance of faecal impaction, it is recommended to use laxatives to make stool soft and easier to pass and encouragement of passing stool regular. In the review, the authors have made an easy overview flow chart of management of childhood constipation, explaining which interventions are needed and what to do if no effect is achieved. For example, if refractory constipation, the authors suggest use of transanal irrigation, botulinum toxin, neuromodulation, and surgical treatments.